Abstract
Background: The management of febrile neutropenia in case of prolonged profound neutropenia remains challenging as there are many possible infectious and non-infectious causes for fever in these patients. In more than 60% of cases there is no documented infectious etiology and unresolved febrile neutropenia often results in multiple empirical modifications of antibacterial therapy and/or addition of antifungal therapy. Unfortunately, indiscriminate use of broad-spectrum antibiotics can lead to important collateral damage including toxicity, selection of multidrug resistant pathogens and an increased predisposition to other infections such as Clostridium difficile or yeasts/fungi. In this study, we investigated whether procalcitonin (PCT) is superior to C-reactive protein (CRP) in discriminating between different etiologies of fever.
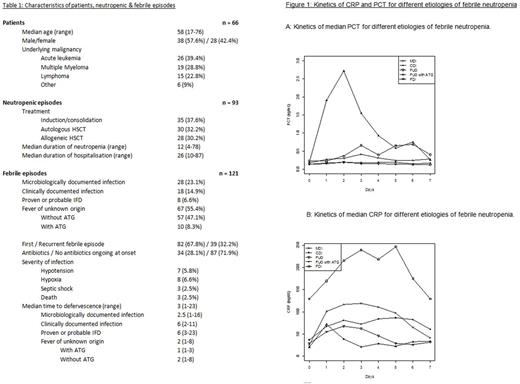
Methods: CRP and PCT were tested daily during 93 neutropenic episodes in 66 patients (Table 1). A linear mixed model was performed to evaluate the effects of different variables on the values of CRP and PCT over time. A total of 121 febrile episodes occurred during this study period and were classified into four categories based on clinical and microbiological findings: microbiologically documented infection (MDI); clinically documented infection (CDI); proven or probable invasive fungal disease (IFD); fever of unknown origin (FUO). The values of PCT and CRP on day 2 after onset of fever were considered for analysis of their performance in distinguishing etiologies of fever in receiver operating characteristic (ROC) curves and by calculation of sensitivity, specificity, positive & negative predictive values and efficiency.
Results: In 61 out of 93 neutropenic episodes (66.7%) the evolution of PCT and CRP was clearly different. CRP seemed to be a more volatile parameter, rising above its ULN (3 mg/dL) during every neutropenic episode. Its reactivity to stimuli was also quite pronounced with a median of 2 surges above 100 mg/dL per neutropenic episode. In contrast, PCT did not rise above its ULN (0.5 ng/mL) in 50 out of 93 neutropenic episodes (53.8%). The only confounding factor on the evolution of CRP and PCT with a clinically relevant large effect size was administration of antithymocyte globulin (ATG), which led to an 11-fold increase of PCT versus a 2-fold increase of CRP.
On the day of fever onset no significant difference in PCT values was observed between different etiologies of fever (p=0.314), whereas median CRP values were significantly higher in IFD versus all other etiologies (median 98.8 mg/dL vs 28.8 mg/dL, p=0.027). Both PCT and CRP reached their peak at a median of 2 days after onset of febrile neutropenia. Median PCT values on day 2 showed no statistically significant difference when comparing etiologies of fever (Figure 1A). There was a tendency towards higher median PCT values in MDI and IFD where they rose > 0.25 ng/mL, while they did not in CDI or FUO without prior administration of ATG. Median CRP values on day 2 after fever onset were significantly higher in IFD versus all other etiologies (median 172 mg/dL vs 78.4 mg/dL, p=0.002). In MDI median CRP values rose > 100 mg/dL, whereas they did not in CDI or FUO (Figure 1B).
The discriminatory power between IFD and FUO of CRP on day 2 after onset of febrile neutropenia was superior to that of PCT. With the cut-off set at 200 mg/dL, CRP has a positive predictive value of 66.7% and a negative predictive value of 97% for the diagnosis of IFD versus FUO, leading to an efficiency of 94.5%.
Conclusions: Both CRP and PCT are not able to predict neither etiology nor severity of infection at the onset of fever. When performing reassessment of antibiotic therapy 2 days after onset of febrile neutropenia, CRP has the better discriminatory power between etiologies of fever and shows higher peak values in clinically severe infections. As such we conclude that PCT has no added value over CRP for clinical management of febrile neutropenia. In our study a CRP value above 200 mg/dL has a positive predictive value of 66.7% and a negative predictive value of 97% for the diagnosis of IFD versus FUO (when MDI and CDI were ruled out by diagnostic workup). A high CRP in the absence of a clear focus of infection might prompt earlier investigation for IFD, leading to earlier treatment initiation and lower mortality. In view of the low numbers of IFD in our study it is important to note that this finding should be confirmed in a larger patient population.
Verlinden: MSD - Merck: Research Funding. Gadisseur: Bayer: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.